NHS
What possible reason could there be for nursing applications to have fallen?
As the FT has reported this morning:
The number of applications to nursing courses at UK universities has fallen sharply, prompting the Royal College of Nursing to call for emergency measures to boost recruitment and address NHS staff shortages.
Apparently, university applications for nursing courses are down 7.4 per cent compared to last year.
This blows a massive hole in the government’s stated plan to recruit more nurses.
It also gives rise to the question ‘why might this be happening?’
Could it be that that treating nurses with contempt and refusing their reasonable pay demands, so forcing them to strike, might have had anything to do with this?
Ministers would deny this, of course.
Anyone with the slightest common sense might express amazement that applications are as high as they are given the shoddy way in which all NHS staff have been treated by this government.
Ministers who think they can score points over state employees without repercussions arising really are very stupid.
And no one believes Wes Streeting will be any better.
Merseysiders protest government moves to replace skilled medics with less skilled
Demonstrations continue against Tory ‘downskilling’ of the NHS to increase profits
Members of the Merseyside Pensioners Association (MPA) joined health workers on Tuesday to protest outside a meeting of the Cheshire and Merseyside Integrated Care (ICS) board meeting against plans to cut NHS costs by reducing skill levels in the health service in a copy of unequal and heavily-privatised US healthcare.
The protest and meeting were held at the Floral Pavilion in Wirral’s New Brighton. The MPA joined a large crowd of Wirral Clinical Support workers and Unison members who have been demanding better pay. MPA members were protesting against the downskilling of medical professionals – a move under the so-called NHS Workforce Plan to replace doctors, midwives, nurses, anaesthetists and other highly-qualified workers with cheaper, less qualified staff to pad NHS staff numbers and reduce wage cost, allowing private health companies to provide services at greater profit.
One MPA campaigner told Skwawkbox:
Forcing or encouraging staff to work beyond their competencies is dangerous for patients and staff. NHS campaigners have been highlighting downskilling, professional deregulation, working beyond competencies and similar government moves for several years. It is not accidental, nor is it a response to “shortages of doctors”, “ageing population “, “bed blocking” or “underfunding” – these terms are all propaganda put out to justify the deliberate systematic destruction and withdrawal of the NHS to benefit big business & increase profit.
Some of us went into the meeting, raised questions about the difficulty and hostile processes involved in booking a GP appointment, the difficulty getting to see an actual GP rather than a Physician Associate [a position carrying out medical duties with only two years’ basic training] or other staff member and the lack of continuity that means we rarely see the same person twice.
We told the Board that we want to see fully-qualified medical professionals, that the right people with the right skills for the right job are fully-qualified doctors, anaesthetists etc. The Assistant CEO told us they have bought a new ‘cloud telephony’ service but that there won’t be any increase in GPs or Practitioners in GP surgeries, therefore we assume no increase in appointments either!
So the response appears to be they’ll just move the deckchairs on the Titanic around in a different manner! A longwinded way of saying they had wasted money on a new phone service presumably so you can more easily be told there are no GP appointments. At the ICS Annual General Meeting/ICB meeting last year an actual GP pointed out that without more GPs/appointments, changing the telephone system wasn’t going to help.
A further campaign meeting will take place on Friday 23 Feb at Liverpool’s socialist bar, the Casa:
The government’s use of ‘associates’ instead of fully-qualified medics has already been linked by coroners to at least two avoidable deaths.
SKWAWKBOX needs your help. The site is provided free of charge but depends on the support of its readers to be viable. If you’d like to help it keep revealing the news as it is and not what the Establishment wants you to hear – and can afford to without hardship – please click here to arrange a one-off or modest monthly donation via PayPal or here to set up a monthly donation via GoCardless (SKWAWKBOX will contact you to confirm the GoCardless amount). Thanks for your solidarity so SKWAWKBOX can keep doing its job.
If you wish to republish this post for non-commercial use, you are welcome to do so – see here for more.
NHS paradigm
There is simply, I fear, nothing to add to this EveryDoctor tweet. We actually have to just wait away:... Read more
As well as us, the government is betraying our children and they are our future
Under the headline ‘Experts Lament the Appalling decline of the health of under fives in the UK’ the Guardian draws attention to the Academy for Medical Sciences report highlighting the widespread obesity and the rampant dental caries in so many of our young. Not only is this harmful for our children, it is also harmful... Read more
GPs in England at ‘Breaking Point’ Amid ‘Collapse in Morale’
Primary care doctors in England are feeling “despondent” and feel unable to provide adequate care given the current pressures on workloads and funding, Byline Times has been told.
GPs and emergency doctors are picking up the pieces amid long waits for operations, as well as a crisis of mental health underfunding, according to testimony shared with this newspaper.
And a significant number of GPs are leaving permanent positions for locum roles (filling in for those ill or on leave), or leaving clinical careers altogether amid unsustainable workloads and heavy admin burdens.
Dr Kath Fielder, a GP in the north-east, told an EveryDoctor survey for Byline Times: “Everyone I know who is a GP is very tired, despondent and weary. I actually think the predominant emotion is sadness. Nothing works like it should and it’s truly heartbreaking seeing patients receiving substandard care from the entire NHS.
“We in primary care have become a holding bay: for people waiting years instead of months for urgent procedures; managing people with significant mental health problems because they aren’t 'bad enough’ to reach the threshold for a massively under-funded CAMHS [Child and Adolescent Mental Health Services]; writing appeals for PIP [Personal Independence Payment] because so many people are losing their benefits.”
She compared the situation to “handing someone a thimbleful of water when their house is on fire”.
“I rarely send patients to hospital but, when I do, I am truly shocked at how many are sent straight home again," she added. "And this is not criticism of the hospital staff. I know they will be under incredible pressure not to admit anyone and there won’t be any beds for them to lie in. Whilst this is happening we are having increasing restrictions in what we can prescribe; where we can refer and impossible targets to attain.”
 Dr Kath Fielder: “Everyone I know who is a GP is very tired, despondent and weary...Nothing works like it should."
Dr Kath Fielder: “Everyone I know who is a GP is very tired, despondent and weary...Nothing works like it should."
Some GPs are now “unable to work” given the conditions, and many more are swapping permanent posts for temporary or ad hoc work.
Asked what the biggest challenges for her practice are right now, she added: “Not being able to give the care we want. It’s that simple.”
Dr Nicholas Souter, a GP based in the south-west, said GP practices had increasingly been incentivised to hire less-qualified Associate Physicians or Advanced Nurse Practitioners (ANPs) over GPs as they were cheaper to employ.
It comes as a new British Medical Association survey of 18,000 doctors found that 55% of respondents said the employment of PAs (physician associates) and AAs (anaesthesia associates) in their workplace had increased their workloads, rather than reduced them.
Just 21% of doctors responding to the survey said the presence of these staff had reduced their workload.
Along with complaints over increased workload, the BMA’s survey also highlighted serious concerns about the use of PAs and AAs regarding patient safety.
Among doctors working in primary care (typically GPs and A&E doctors), 90% told the BMA the way that PAs were being employed in the NHS was a risk to patient safety, with 82% believing PAs frequently or often worked beyond their capabilities.
Dr Souter pointed to a recent case of two ANPs analysing a patient’s bloods, which they said “showed a build up of toxic substances''. One told the elderly patient that her life was under threat and she must go to hospital.
Dr Souter said: “I looked up old bloods and noted this lady had chronic kidney disease.” Her blood toxin levels were always that high – in fact, they were usually higher. “She did not have acute renal failure… So this ANP-to-ANP discussion was all a misunderstanding – the Advanced Nurse Practitioners was reviewing bloods taken by another ANP and neither knew the difference between chronic renal failure and acute renal failure.
"The poor woman was stressed, her family was stressed, an unnecessary ambulance had been sent, an OOH physician had been kept busy.”
The GP said practices should “never” be allowed to have less-trained ANPs outnumbering GPs “but of course, while the Government is under-funding GP practices there is no way to resolve this”.
However, one GP said that recruitment of Physician Associates – which was ramped up following the 2019 Government contract with GPs – followed “years of practices struggling to recruit salaried doctors”.
Another added: “The GP contract has generally speaking buggered up our practice as the funding has not matched the demand. That said, so many factors are making GP a nightmare to work in (and manage) that pulling out one strand is very difficult. PAs in the surgery are very hit and miss. We have had two that have been utter disasters, making more work by wanting constant intervention on the part of their supervisor for the days, having a long list of things they won't do, and referring all kinds of things that don't need referring.
“We have, however, had one who is an absolute legend and has been a pleasure to work with – we wouldn't lose her for the world. The problem is that you don't know what kind you are going to get.”
Six other GPs who spoke to EveryDoctor, and who wished to remain anonymous to speak more freely, echoed these concerns – noting GP practices are struggling to recruit salaried doctors, leading many trainees to choose locum positions for a better work-life balance. This has left full-time partners working extensive hours with additional unpaid admin work.
GPs also pointed to the Government’s 2019 contract with GPs, which they claim has not matched funding with demand.
Several GPs said the current workloads were destroying morale: “On top of my daily appointments, home visits, supervisions, quick reviews, [and] prescribing for the team, I regularly have five to eight sick note requests to action, 50 [test] results and 20 to 30 letters to look at. District nurses tend to send me messages multiple times a day too.
“There has been a huge exodus of GPs in our area so anyone I’m working with is usually newly-qualified. They can’t seem to work at pace, having been trained in the pandemic. I’m frequently having to mop them up too when exhausted or upset over vexatious complaints. Our biggest challenge is retaining GPs because of the above. One has just resigned and is going abroad.
“Morale is terrible. I’m lucky because I have been at my practice for nearly 10 years so most patients are appreciative. But the general public view is we’re rubbish but at the same time want us to do everything/fix everything… and so do secondary [specialist] care.”
In another practice, a doctor described how they have seen a large rise in turnover of GPs: “We have managed to recruit several GPs to replace them… but not in full capacity, because we cannot afford to recruit as many as we need. The new GPs are very recently qualified and so need peer support.”
And they claimed that the recent 6% pay rise for NHS staff in England is not being fully funded by NHS: “[It does] not cover our costs by a long way. Someone at NHS England decided staff costs are about 40% of income. [It’s] more like 60 to 70%. As a result, you are left with a huge dilemma. Our hard-working staff deserve a pay rise but we can't afford it without losing staff to pay for it?”
A&E specialist doctor Dr Huw Evans, based in the West Midlands, said workloads in NHS hospitals meant care expectations had fallen through the floor. His department is constantly under-staffed, with significant vacancies among specialists, he said.
The failure to invest in infrastructure after years of austerity is also visible, with Dr Evans noting: “There are numerous buckets under holes in the roof” of the hospital.
 Dr Huw Evans says buckets fill with water from leaks in his hospital due to crumbling infrastructure
Dr Huw Evans says buckets fill with water from leaks in his hospital due to crumbling infrastructure
“Patients are missing out on the professional relationships that used to be commonplace in the community. As a result, they come to [Emergency Departments] – we never close – where problems that could be dealt with in a few minutes take many hours to sort out."
The breakdown in primary care, including huge delays to get GP appointments, in turn slows down care for those who really need emergency help, he said: “The sight of queued ambulances is the most visible aspect of this. We are not able to offer the level of care that we would wish and have given up on the 'Gold Standard’ aspirations. It used to be that a four-hour breach would cause castigation. Now, any patient who is not a 12-hour breach is a cause for celebration.
“I have worked for the NHS for over 30 years. The NHS is sinking like the Titanic, holed by the iceberg of under-investment. Captain Sunak [is] putting his telescope to his blind eye, telling us he only sees clear water ahead.”
Dr Julia Grace Patterson, EveryDoctor's chief executive, told Byline Times that the Government's "political actions" had "decimated" the NHS.
“NHS GPs are absorbing an enormous amount of pressure currently," she said. "They are doing everything they can to keep patients safe, but this becomes more and more challenging as the situation evolves. The Government is not supporting the current GP workforce, they are often scapegoated for problems that they have not caused, and there is now a move to flood the NHS with non-doctor clinical decision-makers, which is exacerbating the situation.
“Every healthcare professional has a role, and within a fully-functioning NHS with abundant resources, physician associates would be a welcome addition to clinical teams. We definitely hear about some places in the NHS where they are highly valued. However, in many NHS facilities, the burden of responsibility for supervision of their work falls to doctors. This is hugely labour-intensive and even dangerous, given the pressure on the NHS, the rate at which staff must work, and the potential for diagnoses to be missed and patient safety problems to be caused.
“Morale amongst GPs is very low, and the situation must be urgently tackled. The Government must listen to frontline GPs and healthcare leaders to rectify the situation. Politicians are profoundly failing NHS staff and the patients they are devoted to caring for.”
Commenting on concerns over the roll-out of Physician Associates, a Department of Health and Social Care spokesperson said: “The role of Physician Associates is to support doctors, not replace them, and they make a significant contribution to the NHS. PAs work alongside doctors providing medical care as an integral part of the multi-disciplinary team. They carry out clinical duties such as taking medical histories, carrying out physical examinations, and developing and delivering treatment and management plans.
“Regulation of these roles has cross party support and will boost patient safety, with the General Medical Council operating strict fitness-to-practice procedures and setting education and training standards.”
The Government’s Long Term Workforce Plan aims to increase the Physician Associate workforce in England to 10,000 by 2036 to 2037, and the similar Anaesthetic Associate workforce to 2,000 over the same period.
Officials say new regulations will give the General Medical Council responsibility and oversight of doctors, PAs and AAs, allowing it to take a “holistic approach” to the education, training and standards of the roles.
The testimony from GPs and patients was gathered by EveryDoctor
Do you have a story that needs highlighting? Get in touch by emailing josiah@bylinetimes.com
Sunak admits failure
I’m no fan of Morgan but I think this couple of minutes worth highlighting, It is good that Sunak is challenged even by those that that he probably considers likely to give him an easy ride. Morgan adding personal experience made Sunak slightly uncomfortable – though a good deal less than he should have been:... Read more
To claim we cannot afford more health and social care is an outright lie put forward by both the Tory and Labour leaderships, who are only interested in serving the wealthy
The Guardian reports this morning that:
Ministers must urgently inject £4bn into English town hall budgets to head off an “out of control” financial crisis that threatens to drag well-run councils into bankruptcy and put local services at risk, a cross-party group of MPs has warned.
The levelling up, housing and communities committee said government must act now to help councils stricken by shrinking resources and the costs of rising demand for adult social care, child protection, homelessness and special educational needs provision.
I have little doubt that the MPs in question are right. But that will not change Tory policy. And since Labour has accepted Tory sending limits, a general election will change nothing either. Very clearly, the leadership of neither party cares about vulnerable people.
Coincidentally, I noticed this data on the NHS budget from the King's Fund, which is an NHS think-tank:
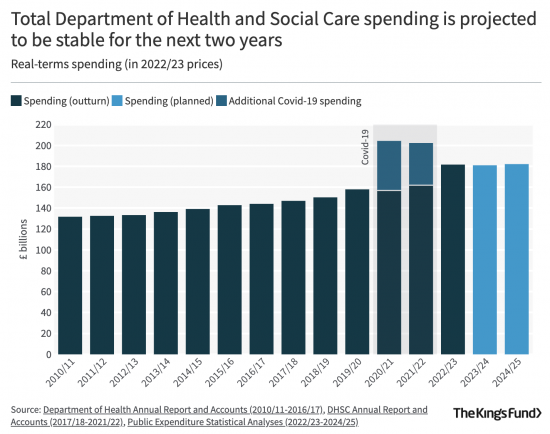
To survive and meet the demand from demographic change as well as fund the increased possibilities that technology provides, the NHS needs real increases in budget of around four per cent a year. It is going to get none in a time of inflation, meaning that real cuts are planned.
These MHS cuts are what are funding Tory tax cuts.
Labour has accepted these tax cuts because they are saying they will live within Tory plans and will not raise taxes.
In other words, there is the clearest evidence, yet again, that a general election will not change anything because the leadership of neither party cares about vulnerable people, as sick people always are.
None of this is necessary, of course. The whole point of writing the Taxing Wealth Report 2024 has been to show that massive sums are available in additional taxes that can be structured to fall almost entirely on the wealthiest, whilst up to £100 billion more can be found for investment by restructuring tax incentivised savings.
We do not need to impose misery on the UK.
We do not need to destroy local democracy.
We do not need to give in to climate change.
There is more than £8,000,000,000,000 of financial wealth in the UK (that's £8 trillion, or £8 million million). To pretend there is no money left is not just absurd; in fact, it is an outright lie.
It is a lie used to support the fact that our leading politicians of both major parties just do not care.
I really do not know for how long the country will put up with this.
Hat tip to Roy Lilley for the link to the NHS data.
Democratising the NHS: Beyond ‘Whatever the Board Wants’
The Thirlwall Inquiry into events at the Countess of Chester Hospital has begun gathering evidence. Later this year, there will be hearings. And careful work to discover how a neonatal nurse killed under her teammates’ noses, while doctors who urged managers to alert the police were ordered to draw a line, attend mediation, and apologise to the colleague they suspected of murdering.
The inquiry will explore the experiences of parents and has statutory powers to compel witnesses to give evidence under oath. It will examine not only the conduct of the board, managers and the medical workforce at the hospital and the role these played, but also the effectiveness of management, governance, and professional regulators throughout the NHS in keeping babies in hospital safe. It will ask whether the accountability of senior managers should be strengthened and consider how NHS culture may need to change. Once it concludes, will the public be safer?
Unlikely. At least, if history is any guide. Letby is the latest inquiry in a twenty-year string running from the Bristol Royal Infirmary children’s heart surgery scandal to the present. The awfulness uncovered in Mid-Staffordshire in 2013 produced an outcry. It led to an NHS-wide review of culture by Sir Robert Francis KC and the appointment of guardians to encourage speaking up.
Supported by an independent national officer, yet fatally on the payroll of local NHS trusts themselves, the guardians were trumpeted as holding boards to account. But they have ended up disappointing, including it seems, Sir Robert who spoke last year of an NHS where staff must “go on strike to get listened to.” Where the culture is “whatever the board wants.”
When higher-ups are the block, what remains? A democratic reset seems a surer way to give patients and workforces a voice than top-down programmes reliant on the character of local leaderships. A paper in the Journal of Medical Ethics by Dr Edwin Jesudason – a consultant in rehabilitation medicine in Scotland – offers some thoughts on how that might work.
Taking an axe to the management fiefdoms that control NHS trusts, the author, a former paediatric surgeon and whistleblower, argues that just as patients must give informed consent to medical procedures, where managers’ decisions can harm, the public should be informed of the risks and have the right to say no. Had managers had to publish the unexplained escalation in deaths at the Countess of Chester Hospital, some babies might have been saved. To put power in people’s hands and broaden decision-making, Jesudason recommends upping the representation of frontline staff and patients on NHS boards and placing term limits on executive appointments. Requiring managers to rotate back to the frontline, he argues, would lessen “us and them divides.”
The paper is a response to an NHS disaster. But its ideas have relevance wherever there are power ingroups and outgroups. In the Post Office, higher-ups exploited private prosecutions and legal muscle to pin IT-generated deficits on blameless sub-postmasters. In healthcare, poor leaders fear bad publicity, hide risks and hijack disciplinary processes, meant as public safeguards, to silence whistleblowers.
Once subjected to motivated allegations, whistleblowers face being put through the wringer of an opaque internal process. Simply for surfacing risks as medical ethics demand. In the best case, investigators may decide the allegations were baseless. But even then, the damage “can be lifelong”, as a 2015 report on regulatory referrals and suspensions noted. Alternatively, a doctor or nurse may emerge with their reputation for competence unblemished, yet still face the sack because the employer says relations have collapsed. Should they seek legal recourse, they must convince a judge that their whistleblowing was why they were dismissed and not the reason argued by the publicly funded big-name lawyers fighting the employer’s corner.
Requests for disclosure will meet with stonewalling, extreme redaction or point-blank refusals dressed up as legal privilege. People may discover that email accounts were deleted or meetings unminuted, only for notes to later surface.
They may even, as in Dr Chris Day’s disclosure-fraught legal marathon, be told an executive has destroyed up to 90,000 emails, but the judge considers “a fair trial is possible and there is no substantial risk of injustice”. Win or lose, the individual will emerge psychologically battered, with a sense, of having “a target on my back”, says the whistleblower Peter Duffy, who was subjected to a two-year investigation by the General Medical Council (GMC), which eventually found there was no case to answer.
Despite promises to “learn lessons” inquiries often lament that again the same mistakes were made. They need not. Rather than chronicling how patients were failed and staff ignored, inquiries should track back to the underlying structures and power relationships that encourage non-consensual leadership and recommend reforms.
Jesudason’s paper offers the Letby inquiry some ideas to work with. These include: “meaningful representation of staff and patients” on boards in place of “placatory consultations.” Also, beefed-up “local democratic oversight” that is not susceptible to board capture – a criticism that campaigners make of today’s councils of governors. Lastly, legal reform to prevent lawyers acting for public institutions from abusing legal privilege to bury risks that the public would want out in the open.
And there are other reform-minded campaigners with ideas that merit attention. One proposal, with widespread medical backing, including by Doctors Association UK and the British International Doctors Association, and a forward by a former NHS England chair, calls for the statutory establishment of independent elected scrutiny panels to ensure disciplinary proceedings are fair. Composed of senior doctors and nurses elected by the workforce, with non-executives representing the board, the panels would guard against miscarriages of justice, says Dr Arun Baksi, an emeritus consultant physician and co-author.
A democratised NHS would help rebuild trust between managers and the healthcare workforce. It would allow public money thrown at lawyers to be spent on patients. In the same way that the sub-postmasters punctured the Post Office’s narrative once they learned of each other’s stories, the pooling of knowledge that democracy enables would make cover-ups harder.
Democracy cannot guarantee good leadership. But when well administered – with safeguards such as modest term limits – it does require leaders to leave their siloes and hear the issues people are raising. Trinity College Dublin, unusually, has a tradition of electing its university provost, deans, and heads of schools. “It gives people some degree of ownership and a voice in what’s going on within their institution,” reflects Louis Brennan, a professor at the university. “That’s the big plus.”
Democracy may not cure the NHS’s accountability crisis. But, as a step towards cultural recovery, it seems a better focus for inquiries than simply rehearsing the ways in which the public has been failed.
Labour front bench takes £650k from health privateers – more than Tories
Starmer and co rake in cash from private health donors – twenty-five percent more than the Tories
Keir Starmer and his front bench MPs have taken almost £650,000 from private health companies, according to a compilation of their declarations of MPs’ interests.
The totals accepted by MPs in Starmer’s Shadow Cabinet between 2020 and 2023 are:
- Keir Starmer £157,500
- Shadow Health Secretary Wes Streeting £193,225
- Shadow Home Secretary Yvette Cooper £231,817
- Shadow Chancellor Rachel Reeves £14,840
- Deputy Labour leader Angela Rayner £50,000
- Shadow Foreign Secretary David Lammy £1,640
- Total £649,022
Figures compiled by David Powell
The total accepted by Labour beats similar donations to the Tories by around twenty-five percent. Starmer and his health spokesman Streeting have vowed to extend the use of private companies for NHS services if Labour gets into government, while promising further austerity and refusing to say they will increase NHS funding to meet need, or increase wages for NHS staff, instead saying – just like Tories – that the NHS must ‘reform’ to be ‘sustainable’.
Both are also fully committed to the ‘Integrated Care’ programme of health rationing and incentivised cuts through withholding care – a direct import from disastrous US healthcare – that is wrecking the NHS even more thoroughly that previous Tory ‘reforms’.
SKWAWKBOX needs your help. The site is provided free of charge but depends on the support of its readers to be viable. If you’d like to help it keep revealing the news as it is and not what the Establishment wants you to hear – and can afford to without hardship – please click here to arrange a one-off or modest monthly donation via PayPal or here to set up a monthly donation via GoCardless (SKWAWKBOX will contact you to confirm the GoCardless amount). Thanks for your solidarity so SKWAWKBOX can keep doing its job.
If you wish to republish this post for non-commercial use, you are welcome to do so – see here for more.
Suppose we got rid of the management pretence that public services can be run by trusts? What would that save?
As the FT notes this morning:
The British government could save at least £20bn a year by modernising IT systems, tackling fraud and getting a grip on failing mega-projects such as the HS2 rail line, according to the head of the UK government’s independent spending watchdog.
To be candid, I really do not doubt it.
But imagine how much more it could save if it stopped pretending that so much of the public sector was made up of independent organisations competing with each other rather than cooperating to provide integrated services.
Take this on the NHS. There are:
- 42 integrated care boards, which each have an integrated care partnerships
- 229 total number of trusts, including 154 foundation trusts
- 50 mental health trusts
- 10 ambulance trusts
- 124 acute trusts
Each of these will spend its life:
- Creating duplicated policy
- Accounting furiously to each other, billing like crazy and employing an army of accountants to reconcile the results
- Have its own PR and comms teams
- Spend a fortune on websites, glossy annual reports and more
- Duplicate management structures
And all for no gain and a lot of cost. Regional strategic health authorities could solve that.
And then there is education, where in 2022 (I struggled to find more up-to-date information quickly), there were 2,539 multi-academy trusts operating in England, made up of nearly 10,000 schools. That still left 17,500 outside trusts, rather surprisingly, but all these trusts suffer all the problems noted above, and destroy the chance of integrated education provision in any area, which should be the goal.
What if we got rid of all this nonsense? What would that save?



